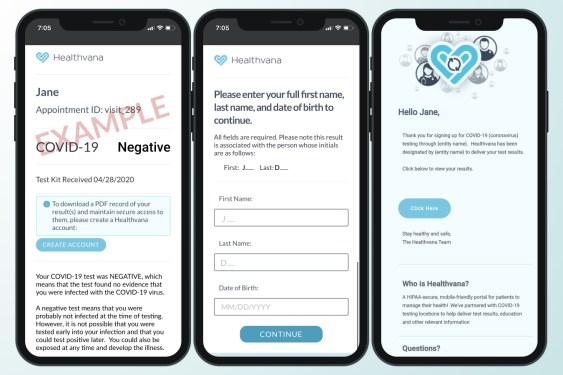
Healthvana’s digital COVID-19 vaccination records are built for patient communication, not immunity credentials
A health-tech initiative is reimagining how vaccination information reaches people, aiming not just to prove immunity but to drive engagement with care. As COVID-19 vaccination campaigns begin to roll out despite a rocky start, an array of companies is stepping in with supportive tools and services. Healthvana, a health-tech startup that originally focused on digital patient information for individuals living with HIV, is enabling Los Angeles County to deploy mobile vaccination records for COVID-19 through Apple’s Wallet technology. A quick read might suggest this is simply about convenient proof of vaccination; however, Healthvana and its collaborators are prioritizing informed participation in personal healthcare, not issuing an immunity passport. The emphasis is on helping people understand their health and participate in care programs, which researchers and clinicians believe can lead to better outcomes and more effective public health interventions. This shift in focus—from mere documentation to meaningful engagement—reflects Healthvana’s broader mission to improve health literacy and adherence to recommended care through user-friendly digital experiences.
Healthvana’s patient-centric approach and the LA County rollout
Healthvana’s approach to healthcare technology begins with a design philosophy that centers on patient engagement and comprehension. The company originally built its platform to support education and communication around HIV, recognizing that traditional channels often fail to reach patients in ways they can easily understand or act upon. The leadership at Healthvana argues that the look and feel of healthcare interfaces have historically resembled outdated software environments, such as Windows 95, which can create friction and hinder patient involvement. In contrast, Healthvana aims for interfaces that resemble consumer-grade social platforms, such as Instagram, to facilitate smoother interactions between patients and their health information. This user-friendly emphasis is not about cosmetic appeal alone; it is about lowering participation barriers so patients engage with care plans, follow-up appointments, and preventive measures more readily. The rationale is that when patients can navigate information in a familiar, intuitive way, they are more likely to act on recommendations and stay connected with care teams.
The company’s velocity in applying this philosophy has been demonstrated by measurable outcomes in HIV care. Bastani notes that patients engaging with Healthvana’s education and communication tools were 7.4 times more likely to attend their next follow-up appointment than those who received follow-up information and appointment notices via traditional means. This statistic highlights the potential impact of patient-facing technology on care continuity, a critical factor in both chronic disease management and acute care pathways. Beyond improving individual outcomes, Healthvana’s model is designed to reduce operational costs for healthcare providers. By streamlining communication and clarifying expectations, the platform aims to cut down on the volume of clarifying calls, login support, and misunderstandings that commonly consume clinician and support staff time. This is achieved through a combination of simplified messaging, clear instructions, and timely reminders that align with patient workflows.
In its partnership with Los Angeles County, Healthvana extends its patient-centric approach to the vaccination phase of the COVID-19 response. The objective is to deliver vitally important information that supports a successful rollout, with particular attention to vaccine schedules and follow-up actions. The partnership emphasizes helping residents stay informed about their vaccination status, including when their two-dose series is complete or when a booster may be due, depending on the vaccine in use. While the platform provides vaccination records via Apple Wallet, its core value proposition remains informing and motivating patients to take necessary steps in their vaccination journey and broader COVID-19 care. It is this emphasis on actionable information—practical steps that patients can take immediately—that underpins Healthvana’s contribution to the public health effort. In practical terms, the system enables a seamless flow of information between the patient, the vaccination event, and the ongoing care pathway, reducing confusion and making it simpler for individuals to stay aligned with recommendations.
Healthvana’s strategy also encompasses a broader vision for healthcare delivery, one that seeks to minimize unnecessary administrative burdens on clinicians and care staff. By compressing the back-and-forth communication that typically fills phones lines and inboxes, Healthvana can free up time for clinicians to focus on direct patient care. Bastani argues that the core principle across healthcare is patient attention and action; without engagement, even the best clinical guidance may fail to translate into improved health outcomes. The LA County deployment embodies this principle by leveraging digital engagement tools to support vaccination uptake while simultaneously addressing follow-ups and care management in a way that scales. The approach is not just about the moment of immunization but about sustaining patient involvement across the care continuum, including the potential for better management of subsequent health needs through informed self-management.
The LA County program also demonstrates how the Healthvana model integrates with existing health systems and workflows. Rather than creating a stand-alone silo, the platform is positioned to complement clinical processes, serving as a layer that communicates essential information in a patient-friendly manner. In practice, this means patients can access vaccination records and related care guidance through a familiar, accessible interface, reducing the cognitive load associated with health information. The partnership leverages Healthvana’s experience in presenting complex medical information in digestible formats, translating clinical concepts into actionable steps for everyday life. By doing so, it seeks to improve adherence to vaccination schedules, increase patient awareness of care options, and sustain engagement across the public health response. The LA County initiative also serves as a potential blueprint for other jurisdictions seeking to combine patient-facing digital health tools with mass vaccination campaigns in a way that respects patient autonomy and privacy.
To expand the reach and impact, Healthvana is pursuing conversations to deploy similar programs in other parts of the country. The drive to export the model reflects confidence in the dual benefits of enhanced patient engagement and reduced administrative strain on healthcare providers. If successful in additional markets, the program could contribute to improved vaccination outcomes nationwide by ensuring that individuals not only receive vaccines but also understand when and why subsequent doses are needed, as well as how to access related care resources. The LA County experience provides a practical demonstration of how digital health tools can be aligned with public health objectives, underscoring the potential for scalable, patient-centered interventions that complement traditional public health messaging and outreach efforts.
Technology design: Apple Wallet integration and the “last mile” of health information
Healthvana’s implementation leverages Apple Wallet to store and deliver COVID-19 immunization records in a digital, portable format. This choice reflects a broader strategy to meet patients where they are, using widely adopted technologies to reduce friction and increase accessibility. The Wallet-based solution is positioned not as an immunization passport but as a convenient repository for vaccine records that patients can carry and present when needed, whether at healthcare facilities, travel checkpoints, or other settings requiring documentation. In essence, the technology acts as a digital extension of the patient’s health information, designed to be easy to use, widely accessible, and integrated with the patient’s daily digital habits. The emphasis on ease of access and clarity aligns with Healthvana’s patient-centric ethos, reinforcing the belief that design choices directly influence health behaviors.
The platform’s broader aim is to deliver timely, relevant, and practical information to patients in formats they understand and trust. Bastani emphasizes that Healthvana is the “last mile” in message delivery—the final step where guidance becomes action. He notes that there are multiple layers involved in determining the proper steps for care and prevention, but the effectiveness of any health intervention depends heavily on how well patients can receive, interpret, and act upon information. In this context, the Wallet integration functions as a convenient touchpoint that communicates vaccination status and related instructions in a format people can access instantly. This immediacy fosters a sense of agency, enabling patients to verify their records quickly and use them when required.
Beyond vaccination proof, Healthvana’s approach includes providing users with information about COVID-19 care and prevention. The system is designed to deliver practical guidance that helps users reduce transmission and manage symptoms if exposure occurs. The emphasis on prevention mirrors a public health priority to curb the spread of the virus by equipping individuals with knowledge about protective measures, testing options, and care pathways. The objective is not only to inform but also to empower people to take appropriate actions in a timely manner. The integration of care information with vaccination records helps create a cohesive user experience, where knowledge about one aspect of health reinforces engagement with other aspects of health management.
From a technical perspective, Healthvana’s Wallet-based records are built to be interoperable with healthcare data standards and existing workflows. While the details of data schemas are not disclosed, the underlying principle is to offer a portable, secure, and user-friendly representation of vaccination history. This approach helps reduce patient confusion about vaccine type, dosing schedule, and timing of doses, while also enabling care teams to verify records quickly. The result is a smoother care continuum, where patients can demonstrate vaccination compliance and clinicians can align clinical decisions with up-to-date information. The Wallet-centric design also aligns with broader trends in digital health, where portable health records and machine-readable data are increasingly used to streamline care coordination and enable timely interventions.
The wallet strategy also supports the initiative’s focus on reducing questions and misunderstandings that often clog clinical workflows. By presenting a concise, verifiable record that patients can reference, the platform minimizes the need for repetitive inquiries about vaccine status and dosing history. This simplification can translate into reduced workload for support staff and clinicians, enabling more efficient use of scarce healthcare resources during a mass vaccination effort. In addition to the record itself, Healthvana’s system emphasizes accessible information about the vaccine, its potential side effects, and guidance on when to seek care. Providing this information in a patient-friendly format fosters better understanding and informed decision-making, aligning with the broader objective of improving health literacy and patient empowerment.
Accessibility considerations are central to Healthvana’s design choices. The platform’s emphasis on a familiar user experience is aimed at broadening reach across diverse populations, including those who may be less comfortable with traditional healthcare communications. By adopting an interface style akin to popular consumer apps, the system lowers the barriers to engagement, encouraging a wider range of patients to access their records, review care guidance, and consider recommended actions. This approach aligns with public health goals of broad participation and equitable access to health information. The Wallet-based records also support privacy and security considerations, as digital records can be stored securely on devices and shared selectively with providers, subject to user consent and device-level protections. The outcome is a patient-centered solution that blends practical usability, data accessibility, and privacy-conscious design—key ingredients for successful deployment in a large public health program.
In practice, the LA County rollout combines the Wallet-record delivery with Healthvana’s broader content strategy, which includes information about COVID-19 care and prevention. The intention is to empower users with knowledge that supports responsible behaviors, such as adherence to vaccination schedules, understanding booster timing, recognizing symptoms, seeking testing when appropriate, and following guidance to reduce the spread. The Wallet integration is thus part of a larger ecosystem designed to improve outcomes by ensuring that people not only have records but also understand what actions to take next. It reflects a comprehensive approach to public health information dissemination, where digital tools complement in-person care and traditional outreach.
Technology and design choices like these can influence the speed and effectiveness of public health responses. The combination of reminders, clear explanations, and accessible records is intended to improve user engagement with vaccination programs and associated care pathways. As such, Healthvana’s strategy illustrates how thoughtful UX, grounded in patient needs, can translate into tangible health benefits. The wallet-centric model demonstrates that digital health tools can be woven into everyday technologies, making it easier for individuals to access critical information without requiring complicated navigation or specialized technical knowledge. The net effect is a more responsive, patient-centered approach to managing immunization records and related health information, with potential spillover effects on broader health outcomes.
Reducing cost and friction for healthcare providers
Healthvana’s impact extends beyond patient engagement to the economics of care delivery. By simplifying how patients receive and interpret their health information, the platform can reduce the volume of time clinicians and support staff spend answering questions, clarifying misunderstandings, and following up on patient concerns. Bastani emphasizes that a major benefit of simpler, more intuitive information delivery is a substantial reduction in “cost to healthcare providers.” When patients can log in easily, understand their results, and comprehend what steps they need to take, there is less demand for phone calls to clarify terms like “SARS nonreactive” or “what does my result mean?” The cumulative effect of these reductions is a notable saving in clinician and care staff hours—resources that can be redirected toward direct patient care and more complex tasks. In an era of stretched healthcare systems, such savings are not merely financial; they can translate into improved access, shorter wait times, and better overall patient experiences.
The LA County initiative leverages these principles, aiming to streamline vaccination workflow while ensuring that residents stay informed about their immunization status. A critical dimension of this effort is eliminating avoidable communication bottlenecks that typically arise during mass vaccination campaigns. By delivering clear instructions and timely updates directly to patients’ devices, Healthvana mitigates a range of common issues that would otherwise consume staff time—log-in difficulties, misinterpretations of test results, confusion about dosing schedules, and delays caused by logistical questions. The net effect is a more efficient vaccination rollout with fewer operational frictions, enabling healthcare facilities to allocate staff and resources to clinical tasks that require direct medical expertise.
Beyond immediate cost savings, the platform’s design supports long-term efficiency gains. For example, by providing standardized, digital records, the system can reduce the administrative overhead associated with paper-based documentation and manual record reconciliation. Digital vaccination records can be retrieved quickly by patients and providers, facilitating smoother verification processes when vaccine documentation is required for travel, school, or employment. In addition, Healthvana’s patient education components help reduce repeat inquiries by equipping patients with better foundational knowledge about vaccines, care pathways, and follow-up requirements. The combination of reduced call volume, faster patient self-service, and improved adherence to follow-up instructions can yield meaningful improvements in operational efficiency and care outcomes.
Healthvana’s cost-reduction message also resonates with the broader health system’s pursuit of value-based care. By fostering adherence to dosages and follow-up appointments, the platform supports more effective use of resources and potentially reduces downstream healthcare costs that arise from missed follow-ups or delayed care. The LA County program thus aligns patient engagement with provider-facing objectives, delivering a dual benefit: empowering patients and alleviating some of the administrative burdens that strain clinics and public health departments during large-scale vaccination efforts. The result is a model in which technology, design, and clinical workflows converge to create more sustainable, patient-centered care that can be scaled to other regions as vaccination campaigns expand nationally.
Performance metrics available from the LA County experience illustrate tangible outcomes. In a relatively short period, Healthvana’s approach to message delivery and patient information sharing has demonstrated its potential to affect public health outcomes by enhancing follow-up rates and improving adherence to vaccination schedules. The combination of user-friendly interfaces, targeted health content, and accessible records helps drive engagement and action at individual levels, which cumulatively contributes to more effective vaccination campaigns and broader disease control measures. The ongoing development of Healthvana’s platform, including potential enhancements to messaging, care guidance, and record interoperability, may yield further improvements in both patient experiences and healthcare system efficiency as more jurisdictions adopt similar models.
Contact tracing and exposure notification: real-world impact vs. native apps
One of the notable outcomes of Healthvana’s patient-centric approach is its contribution to contact tracing and exposure notification efforts. By enabling users to receive timely information about potential exposures and to access relevant testing resources, Healthvana supports a key public health goal: slowing the spread of the virus through timely identification and notification of exposed individuals. Bastani notes that in the greater Los Angeles area, the platform’s deployment over a period of less than two months has resulted in more than 12,000 people being notified that they have been exposed. This figure underscores the potential impact of deploying user-friendly, privacy-conscious tools that facilitate rapid risk communication and prompt action by individuals and households. The ability to notify close contacts quickly creates a ripple effect, enabling families and communities to take protective steps, seek testing, and reduce transmission chains.
The broader context includes an ongoing discussion about exposure notification tools embedded in mobile operating systems. Apple and Google collaborated to release a framework and sample code for exposure-notification apps, emphasizing user privacy and security. While these native tools are designed to enable exposure alerts and protect user privacy, their uptake has been uneven. In some jurisdictions, the adoption of exposure-notification features has not reached widespread engagement levels, despite the robustness of the underlying technology. For example, in Virginia, a state using the exposure-notification framework, only 388 people had sent alerts through the app within three months of its launch. This relatively slow uptake highlights a potential limitation of relying solely on native exposure notification tools to achieve broad public health impact.
In contrast, Healthvana’s approach capitalizes on a direct, user-facing workflow that emphasizes timely information delivery and practical next steps. By presenting users with actionable guidance and access to resources through a familiar digital interface, the platform can drive behavior change that complements the broader exposure notification ecosystem. The LA County experience demonstrates that a patient-centric channel can yield measurable outcomes in terms of contact tracing and risk communication, especially when deployed in a real-world, large-scale setting. The results suggest that while native exposure notification tools are valuable for privacy-preserving risk alerts, augmenting them with accessible, user-friendly health information platforms can enhance overall effectiveness by encouraging users to seek testing, vaccination, or care as needed.
The contrast between Healthvana’s data points and the uptake patterns of native exposure notification features also highlights important considerations for policy and technology design. The volume and speed of notifications, the ease with which people can act on alerts, and the availability of supportive resources all influence the practical impact of exposure notification programs. Healthvana’s model demonstrates how integrated health information delivery and care guidance can operate in concert with exposure notification frameworks to produce meaningful public health benefits. This integrated approach may inform future iterations of digital health strategies, encouraging collaboration among public health authorities, healthcare providers, and technology platforms to optimize outcomes in outbreaks and vaccination campaigns.
Healthvana’s ongoing discussions about expanding similar programs to additional markets reflect confidence in the scalability and adaptability of their model. If adopted in other jurisdictions, the platform could play a role in enhancing vaccination uptake, improving care follow-up, and supporting contact tracing efforts across diverse populations. The potential to tailor content and reminders to regional vaccination schedules, testing resources, and local care pathways could amplify the effectiveness of these tools. Moreover, the ability to deliver targeted health information in a digestible format remains a central strength of Healthvana’s approach, offering a practical pathway to improve health literacy and empower individuals to take informed actions during public health emergencies.
The broader context: native exposure tools versus patient-centered engagement
The comparison between Healthvana’s patient-facing approach and the native exposure-notification tools embedded in iOS and Android devices provides a useful lens for evaluating how digital health interventions influence public health outcomes. Native exposure notification frameworks are built with a strong emphasis on privacy and decoupled data sharing, designed to alert users about potential exposure without revealing sensitive information. While this architecture ensures privacy, the adoption rate—though seemingly modest in certain jurisdictions—suggests that software technology alone is not sufficient to maximize impact. Behavioral factors, accessibility, and the availability of actionable guidance all shape whether people respond to exposure alerts with subsequent testing and preventive measures.
Healthvana’s model, by contrast, foregrounds clarity, immediacy, and practical steps. The design prioritizes straightforward messaging about exposure, testing options, and preventive measures, delivered through a medium that people already use daily. This strategy reduces the cognitive load required to interpret an alert and decide on the next action, which is crucial when time-sensitive decisions are involved. The LA County experience suggests that a combined approach—where native exposure notification frameworks are complemented by user-friendly health information platforms—may yield stronger public health outcomes. In this view, technology serves not only to alert but to guide and support individuals in making informed decisions during an outbreak or vaccination campaign.
The gap between exposure notification uptake and the real-world impact on transmission is an area ripe for further study. Researchers and policymakers are interested in understanding how different digital health interventions influence testing behaviors, vaccination adherence, and adherence to isolation or quarantine guidelines. Healthvana’s experience offers a concrete example of how patient-facing applications can catalyze action by delivering information in an accessible way and connecting users to resources. The real-world effectiveness of such approaches hinges on consistent messaging, reliable access to testing and care, and ongoing engagement with patients across the disease trajectory. The LA County deployment demonstrates that when digital health tools are designed with patient needs in mind, they can contribute meaningfully to both disease containment and health system efficiency.
While the Trail of evidence from Healthvana’s LA County program is compelling, it is important to acknowledge that outcomes will vary across different communities and healthcare ecosystems. Factors such as digital literacy, smartphone access, language barriers, cultural norms, and local vaccination infrastructure all influence the effectiveness of digital health interventions. The ongoing expansion of Healthvana’s model to other jurisdictions will provide valuable data on how well the approach translates across regions with different demographics and health system configurations. The convergence of patient education, record portability, and actionable care guidance may prove to be a versatile framework for improving health outcomes beyond COVID-19, offering a blueprint for patient-centered digital health tools that can be adapted to diverse public health needs.
Expansion potential and implications for national vaccination outcomes
Healthvana’s LA County program represents a testbed for a broader, scalable strategy that could influence national vaccination outcomes and how communities manage COVID-19 care. The combination of immunization records delivered through Apple Wallet, patient education content, and streamlined care guidance addresses several critical pain points in vaccination campaigns: accessibility, comprehension, adherence, and efficient care navigation. If the approach proves effective in a large urban jurisdiction, health systems across the country may consider adopting similar models to support their vaccination efforts and subsequent care processes. The ability to port vaccination records between providers and settings, without friction, could streamline administrative tasks and improve continuity of care for patients who receive vaccines at different sites or in different counties. This flexibility can be especially valuable in periods when vaccine supply and distribution channels vary, requiring adaptable workflows that still preserve patient privacy and security.
One of the core benefits of Healthvana’s approach is its emphasis on patient engagement as a driver of health outcomes. The platform’s design aims to make health information more accessible and relatable, enabling patients to act on recommendations and follow through with care plans. In the context of vaccination campaigns, this translates into better timing for second-dose administration, booster considerations, and retrieval of related care resources. The potential upshot is a more efficient vaccination rollout with higher completion rates and more consistent adherence to preventive measures. Such improvements can contribute to stronger population-level immunity and more resilient health systems during the course of a pandemic and beyond.
The initiative’s focus on reducing the burden on healthcare providers—by minimizing repetitive inquiries and clarifications—also has important implications for healthcare labor dynamics. As clinics and public health departments navigate surges in demand during vaccination campaigns or outbreaks, tools that streamline information delivery and patient self-service can help maintain access to care without overextending staff. In turn, reduced administrative overhead can free clinicians to concentrate on direct patient care, diagnostics, and treatment decisions, enhancing overall care quality during critical periods.
National expansion would require careful tailoring to each jurisdiction’s vaccination protocols, record-keeping standards, and patient population characteristics. Localization efforts would likely include translating educational content into multiple languages, adapting dosing schedules to vaccine types available in a region, and aligning with local public health guidance. The ability to maintain consistent, accurate information across jurisdictions would be essential to ensure trust and effectiveness. As Healthvana and similar platforms scale, interoperability with state immunization registries, clinical information systems, and nationwide health data standards would be crucial to enable seamless data exchange while upholding privacy and security requirements.
The potential for cross-state or cross-market adoption raises considerations about data governance and consent management. Patients must retain control over who can access their records and under what circumstances, which calls for clear consent workflows and user-friendly privacy controls. The balance between data utility for public health and individual privacy is a central theme in digital health deployment. Healthvana’s approach, centered on patient empowerment within a privacy-conscious design, aligns with this balance. As more jurisdictions evaluate digital health tools to support vaccination campaigns and care pathways, the LA County model could serve as a practical reference point for designing, implementing, and evaluating similar programs.
In addition to vaccination-related outcomes, the platform’s broader health education and care guidance features may contribute to improved management of other health conditions. For populations living with chronic illnesses or those requiring ongoing monitoring, patient-centered digital tools that present information clearly and facilitate engagement can make a meaningful difference in adherence to treatment plans and follow-up schedules. If Healthvana expands beyond COVID-19 to address other immunization needs, chronic disease management, and preventive care, the cumulative impact on public health could be substantial. The integration of records, education, and actionable guidance has the potential to create a more proactive health system—one in which patients are equipped with knowledge and resources to participate actively in their own care.
The LA County experience and the broader strategic considerations around digital health tools for public health illustrate how technology, design, and clinical workflow can be harmonized to achieve outcomes that matter for patients and providers alike. As digital health ecosystems evolve, the value of patient-centered, action-oriented information delivery becomes increasingly evident. Healthvana’s model offers a concrete example of how consumer-grade UX principles can be harnessed to support public health goals, reduce administrative friction, and empower individuals to take meaningful steps in managing their health. The ongoing exploration of this approach in different contexts will shed light on the most effective configurations for scaling such tools in support of vaccination efforts, care continuity, and population health management across the country.
What this means for patients, clinics, and public health
For patients, Healthvana’s LA County program offers a tangible improvement in how vaccination information and related care guidance are accessed and used. The Wallet-based vaccination records provide a portable, convenient way to carry proof of vaccination, reducing the hassle of searching for paper records or pulling up electronic documents across multiple systems. The integration of care guidance and prevention information complements the records, enabling patients to understand not just that they were vaccinated but also what steps they should take next—whether it is scheduling a follow-up dose, seeking testing, or adopting protective measures to slow transmission. The user experience is designed to minimize friction, making it easier for people to engage with their health data and act on it promptly. This is particularly valuable for populations that may face barriers to traditional health communications, including those with limited access to healthcare facilities, language differences, or limited health literacy. While the wallet-based approach is not a substitute for in-person care, it acts as a facilitator that helps connect patients with the information and resources they need in a timely and accessible way.
Clinics and health systems stand to benefit from reduced administrative noise and improved patient engagement. By providing a streamlined channel for communicating vaccination records, appointment reminders, and care guidance, the platform can help clinics manage patient flows more efficiently. The potential reductions in inbound calls and clarifications free up staff time for more complex tasks, such as clinical assessment, vaccination administration, and patient education on broader health topics. This reallocation of resources can contribute to more efficient clinic operations, quicker turnarounds for patient needs, and a more positive patient experience overall. At scale, the approach can help health systems better manage peak demand periods during outbreaks or vaccination campaigns, when patient volumes are high and the need for timely, accurate information becomes critical.
Public health officials may view Healthvana’s model as a useful complement to existing strategies for vaccine dissemination, patient outreach, and contact tracing. The ability to notify exposed individuals and to guide them to testing resources in a privacy-conscious manner aligns with efforts to contain the spread of COVID-19 and other infectious diseases. The real-world results observed in LA County—thousands of exposure notifications in a short period—underscore the potential impact of readily accessible, actionable information at the point of care and in personal devices. The approach also emphasizes personal responsibility and informed decision-making, encouraging people to take proactive steps to protect themselves and others. As policymakers consider future digital health interventions, the LA County example provides a practical demonstration of how patient-centric design, record portability, and care guidance can contribute to more effective public health responses.
From a communications perspective, the adoption of Healthvana’s approach can help public health organizations craft clearer, more actionable messaging around vaccination and care. The emphasis on user-friendly information can improve comprehension and retention of important instructions, supporting better health outcomes. In addition, the integration of digital records with everyday devices creates continuity across settings, enabling patients to present trustworthy, up-to-date information when interacting with different providers. This continuity is essential in large-scale vaccination efforts that involve multiple sites and changing guidelines over time. If other jurisdictions replicate this model, the cumulative effect could be a more coherent national strategy that improves patient adherence to vaccination schedules, enhances care coordination, and strengthens the public health response.
The LA County experience also highlights the importance of ongoing evaluation and iteration in rolling out digital health tools. Continuous monitoring of how patients interact with the platform, how often they access records, and how effectively the information translates into action will inform refinements to the system. Metrics such as follow-up appointment adherence, receipt of second-dose reminders, and uptake of testing resources in the event of exposure will be valuable indicators of success. By embracing a data-driven approach to optimization, Healthvana and partner organizations can adapt to evolving public health needs and patient expectations, ensuring that the technology remains relevant, accessible, and impactful as vaccination campaigns progress and new health challenges arise.
In summary, Healthvana’s LA County COVID-19 immunization records program, delivered through Apple Wallet and complemented by clear education and care guidance, represents a strategic integration of patient-centered design with public health objectives. The initiative is not merely about digital records but about empowering patients to participate meaningfully in their health journeys. By reducing administrative friction, supporting follow-up adherence, and reinforcing preventive care behaviors, this model has the potential to influence vaccination outcomes and care engagement on a broader scale. The approach aligns with a growing recognition in healthcare that technology must be human-centered, accessible, and purpose-built to support real-world health improvements. As more jurisdictions explore similar programs, the lessons learned from Los Angeles could inform the design of scalable, patient-first digital health solutions that enhance public health preparedness, response, and resilience in the face of current and future health challenges.
Conclusion
Healthvana’s collaboration with Los Angeles County showcases how patient-centered digital health tools can support a large-scale vaccination effort while simultaneously reducing provider burdens and improving care engagement. By delivering immunization records through a familiar mobile wallet format and pairing this with accessible education and care guidance, the program prioritizes patient action and health literacy alongside records management. The approach emphasizes the importance of user experience in driving meaningful health outcomes, illustrating how “last mile” communications can translate into higher follow-up rates, better adherence to vaccination schedules, and more efficient care delivery. The LA County deployment also demonstrates the potential for digital health tools to contribute to contact tracing and exposure notification efforts, complementing native system capabilities with practical, actionable steps for patients. As the model expands to other jurisdictions, it could help shape national vaccination strategies by providing a scalable, patient-centered framework that improves information accessibility, care coordination, and public health outcomes. The ongoing experience from this program will inform best practices for integrating digital health platforms into mass vaccination campaigns, with implications for future public health initiatives and the broader evolution of patient-centered care.